If you experience leg pain following mild or rigorous activity it may be attributed to Peripheral Artery Disease (PAD), which affects millions of Americans. Poor blood circulation in the legs can cause pain during exercise or periods of rest. There are a variety of contributing factors for PAD, but the primary cause is a narrowing of the blood vessel caused by a buildup of fatty plaque called atherosclerosis. This disease is on the rise so much that the entire month of September is devoted to PAD awareness.

The reason that diagnosing PAD, also known as Peripheral Vascular Disease (PVD), is important is that its progression can cause serious health issues. It can lead to critical limb ischemia, which can exacerbate open wounds, injuries, and infections that do not heal or lead to tissue decay and limb amputation. The disease can also increase heart attack and stroke risk.
Some of the factors that increase the risk for PAD are:
As blood pulses away from the heart, it passes through a network of arteries and smaller blood vessels. If blood flow becomes obstructed, muscles and tissues can be deprived of essential oxygen and nourishment. At rest, a low blood flow may be adequate, but with increased muscle activity the demand for oxygen-rich blood is increased. This may result in muscle pain or cramps, called claudication.
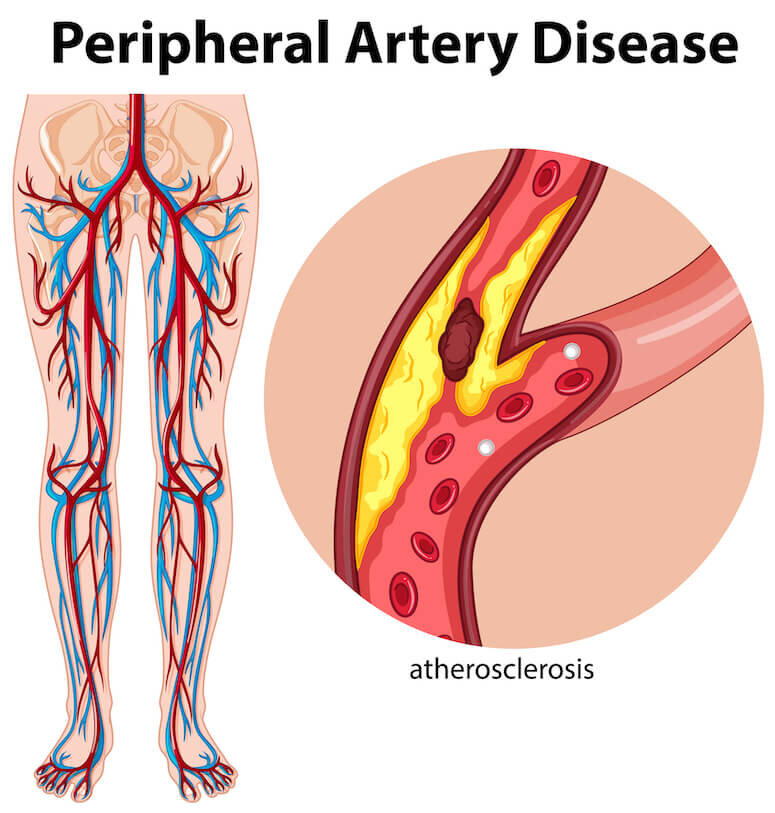
Peripheral Artery Disease most commonly occurs in the legs, but can also present in the arms, stomach, and head. A similar disease occurring near the heart is called Coronary Artery Disease (CAD). Other causes of PAD besides plaque buildup can be inflammation of blood vessels, limb injury, abnormality of ligaments or muscles, or exposure to radiation.
Unfortunately, there are a variety of other issues that can cause leg pain and the disease is often misdiagnosed. Besides wounds and infections, common symptoms include:
While most commonly occurring during exertion, these symptoms can take place during periods of rest, including sleep. Sometimes PAD presents no symptoms.
The ankle brachial index is a test for PAD that measures the difference between the blood pressure in your arm against that near your ankle. Imaging tests may also be performed by a doctor, such as an ultrasound, magnetic resonance angiography (MRA), or computed tomographic (CT) angiography to detect the disease.
Steps can be taken to reduce the buildup of arterial plaque and the risk of Peripheral Artery Disease. Regular exercise, an active lifestyle, a healthy diet, and abstention from smoking diminish the risk of PAD and contribute to good overall health.
There is a range of medical options available depending on the condition and severity of the PAD. Medicines may be used to effectively reduce the causes and effects of arterial blockage if time allows.
Medical management of the disease can include controlling diabetes, losing weight, lowering cholesterol, and reducing blood pressure.
There are multiple minimally invasive endovascular options for treating PAD. These non-surgical procedures are typically performed utilizing a small catheter inserted into the blood vessel. Angioplasty is a common method involving the inflation of a tiny balloon inside the vessel to widen the passageway. A tubular metallic mesh stent can also be inserted into the affected area to expand the blood vessel. Another process uses a laser to remove plaque buildup.
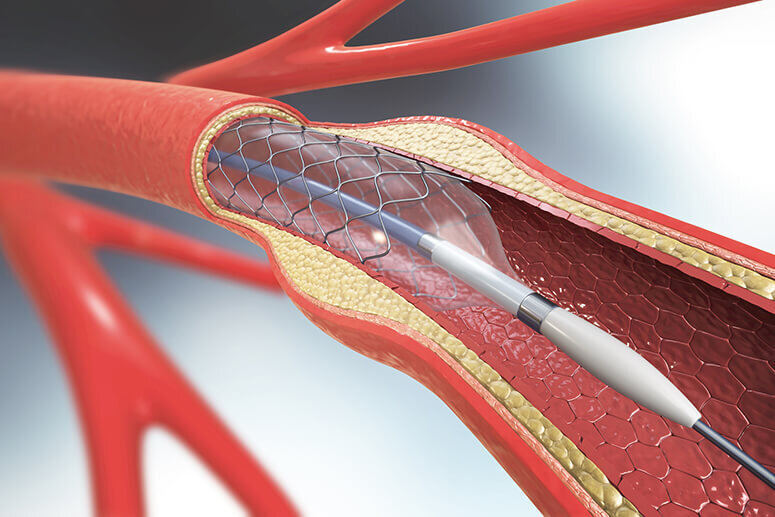
If the Peripheral Artery Disease cannot be managed or treated through minimally invasive procedures, surgery may be required. This determination is also made based on the patient’s risk factors and the length of the blockage, called lesions. Some lesions are too large to be effectively treated through angioplasty, stents, or lasers.
Surgical bypass uses a synthetic material or a segment of a healthy artery from the patient to create a passage around a blocked or occluded artery. Blood flow is rerouted through the new unblocked passageway.
Advancements are continually made in the medical field. An experienced and well-informed doctor can best consult on your individual course of treatment. A board-certified vascular surgeon is ideally suited to diagnose and treat your Peripheral Artery Disease.
In Florida, patients have access to Dr. Christopher Boyes MD FACS for their vascular treatment. In addition to serving as an attending physician at Palm Beach Gardens Medical Center and Jupiter Medical Center, Dr. Boyes consults at Coastal Vein and Vascular Specialists, a private practice in Palm Beach Gardens, Florida.
If you need a consultation or another opinion, contact his office online to schedule an appointment or call 561-295-4110 today.
RESOURCES:
Peripheral Arterial Disease (PAD)
Centers for Disease Control and Prevention
https://www.cdc.gov/heartdisease/PAD.htm
Peripheral Artery Disease (PAD)
Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557
About Peripheral Artery Disease (PAD)
American Heart Association
https://www.heart.org/en/health-topics/peripheral-artery-disease/about-peripheral-artery-disease-pad
How is PAD Treated?
Johns Hopkins Medicine
https://www.hopkinsmedicine.org/heart_vascular_institute/media/video/transcriptions/how_is_pad_treated.html
Subscribe to our newsletter
© Copyright 2023 Coastal Vein & Vascular | All Rights Reserved | Privacy Policy | Powered by Cord Media